Future of Tinea Vaccines
Fungal Infections Can’t Be Prevented by Vaccines (Yet)
Vaccines have been one of the greatest achievements in modern medicine, protecting millions from diseases caused by bacteria and viruses. So why don’t we have a vaccine for common fungal infections like tinea? The answer lies in the complex biology of fungi and the unique ways they interact with the human immune system. This page explores why fungal infections are so difficult to prevent with vaccines—and the future possibilities for overcoming these challenges.
Don’t wait for vaccines—take action now. Real Good Honey Jarrah TA35+ is natural, effective, and fungi aren’t resistant to it.
The Immune System vs Fungi
Dermatophytes, the fungi responsible for tinea, have evolved to suppress and evade local immune responses. When dermatophytes invade the skin, they release molecules that disrupt immune signalling, effectively “hiding” from the body’s defences. This is why fungal infections often linger, as the immune system struggles to identify and eliminate the fungi.
Unlike bacteria and viruses, which trigger robust and long-lasting immune responses, fungi do not elicit strong immune memory. Once the body clears a fungal infection, it doesn’t “remember” how to fight it effectively in the future. Think of it like a student who crams for an exam but forgets everything afterward—the immune system learns how to fight the infection temporarily but doesn’t retain the knowledge.
Fungi hide from your immune system, but they can’t hide from Real Good Honey. Discover a natural solution that works.

The Biological Complexity of Fungi
Fungi are more closely related to humans than bacteria or viruses, which complicates the development of treatments or vaccines. Both fungi and human cells are eukaryotic, meaning they share many cellular structures and processes. So, targeting fungal cells without harming human cells is like trying to eliminate weeds in a garden without damaging the flowers—it’s incredibly difficult.
Tinea can be caused by various species of dermatophytes, each with subtle differences in biology. So developing a universal vaccine that works against all these fungal species is a significant scientific hurdle.
Nature’s complexity calls for nature’s solution. Real Good Honey is powerful yet gentle on your skin.

Why Haven’t We Solved This Problem Yet?
Limited Research Funding:
While fungal infections like tinea affect millions worldwide, they are often seen as non-life-threatening. This perception limits research funding compared to diseases like cancer or influenza.
Focus on Treatment, Not Prevention:
Most fungal research focuses on antifungal treatments rather than vaccines. Current treatments aim to manage infections with topical or oral antifungals, but these often fail to prevent recurrence or reinfection.
The Future of Fungal Vaccines
Scientists are working to identify fungal proteins that could serve as targets for a vaccine, stimulating the immune system to recognise and attack fungi. Research into adjuvants—substances that enhance the immune response—could help overcome fungi’s ability to evade detection. The challenge lies in the diversity of dermatophyte microbes and their ability to suppress immune responses. A vaccine would need to provide broad protection without causing damage to human tissues—a delicate balance.
Start healing with Real Good Honey.
Hope on the Horizon
Experimental vaccines for other fungal infections, such as Candida and Aspergillus, are showing promise. These vaccines are designed to overcome fungi’s immune evasion tactics and could pave the way for vaccines targeting dermatophytes like those causing tinea. Researchers are also exploring genetic and mRNA-based technologies (similar to those used in COVID-19 vaccines) to create highly specific and adaptable fungal vaccines.
While vaccines for fungal infections remain a future goal, advancements in antifungal treatments are currently the best way to manage and control infections. Innovations like Real Good Honey’s hydrogen peroxide honey are designed to tackle fungal infections at their source by breaking down spores and preventing reinfection.
Tackle Tinea spores at their source
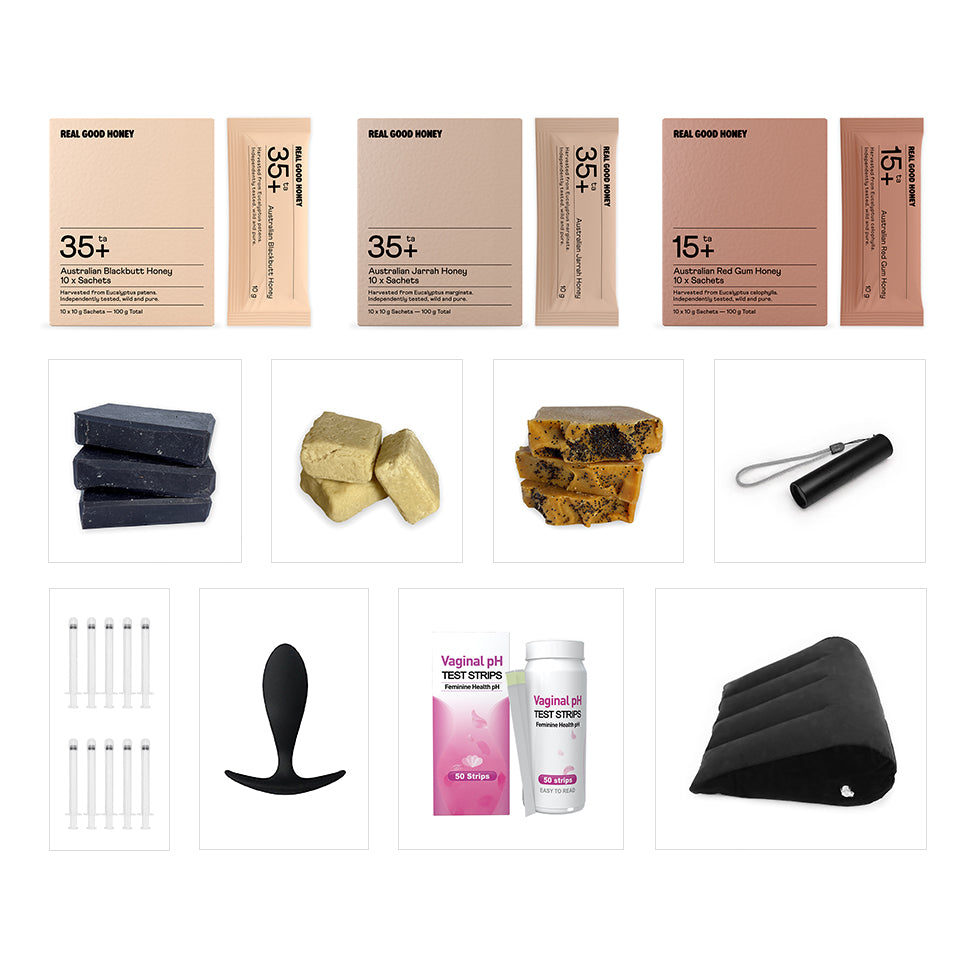

How To Apply Real Good Honey
Mix 1 tsp of Jarrah TA35+ with 1 tsp of sorbolene cream until well combined. Apply the mixture onto the affected area. A minimum 2-hour treatment time is recommended but leaving on for longer is advantageous as the honey will continue to release hydrogen peroxide for up to 24 hours. Covering the treated area with clothing is optional (i.e. socks, gloves, clothing) is optional. Repeat daily for 14 days, or until symptoms have resolved. A maintenance application is recommended to reduce the risk of reinfection from infected sources and organic matter. If symptoms persist or worsen, consult your GP.